Ventricular Septal Defect (VSD)
What Are Holes in the Heart?
Holes in the heart are simple congenital (kon-JEN-ih-tal) heart defects. Congenital heart defects are problems with the heart's structure that are present at birth. These defects change the normal flow of blood through the heart.
Your heart has two sides, separated by an inner wall called the septum. With each heartbeat, the right side of your heart receives oxygen-poor blood from your body and pumps it to your lungs. The left side of your heart receives oxygen-rich blood from your lungs and pumps it to your body.
The septum prevents mixing of blood between the two sides of the heart. However, some babies are born with holes in the upper or lower septum.
A hole in the septum between the heart's two upper chambers is called an atrial septal defect (ASD). A hole in the septum between the heart's two lower chambers is called a ventricular septal defect (VSD).
ASDs and VSDs allow blood to pass from the left side of the heart to the right side. This means that oxygen-rich blood can mix with oxygen-poor blood. As a result, some oxygen-rich blood is pumped to the lungs instead of out to the body.
Over the past few decades, the diagnosis and treatment of ASDs and VSDs have greatly improved. Children who have simple congenital heart defects can survive to adulthood and live normal, active, and productive lives because their heart defects close on their own or have been repaired.
How the Heart Works
To understand holes in the heart, it's helpful to know how a healthy heart works. Your child's heart is a muscle about the size of his or her fist. The heart works like a pump and beats 100,000 times a day.
The heart has two sides, separated by an inner wall called the septum. The right side of the heart pumps blood to the lungs to pick up oxygen. Then, oxygen-rich blood returns from the lungs to the left side of the heart, and the left side pumps it to the body.
The heart has four chambers and four valves and is connected to various blood vessels. Veins are the blood vessels that carry blood from the body to the heart. Arteries are the blood vessels that carry blood away from the heart to the body.
A Healthy Heart Cross-Section
The illustration shows a cross-section of a healthy heart and its inside structures. The blue arrow shows the direction in which oxygen-poor blood flows from the body to the lungs. The red arrow shows the direction in which oxygen-rich blood flows from the lungs to the rest of the body.
Heart Chambers
The heart has four chambers or "rooms."
- The atria (AY-tree-uh) are the two upper chambers that collect blood as it comes into the heart.
- The ventricles (VEN-trih-kuhls) are the two lower chambers that pump blood out of the heart to the lungs or other parts of the body.
Heart Valves
Four valves control the flow of blood from the atria to the ventricles and from the ventricles into the two large arteries connected to the heart.
- The tricuspid (tri-CUSS-pid) valve is in the right side of the heart, between the right atrium and the right ventricle.
- The pulmonary (PULL-mun-ary) valve is in the right side of the heart, between the right ventricle and the entrance to the pulmonary artery, which carries blood to the lungs.
- The mitral (MI-trul) valve is in the left side of the heart, between the left atrium and the left ventricle.
- The aortic (ay-OR-tik) valve is in the left side of the heart, between the left ventricle and the entrance to the aorta, the artery that carries blood to the body.
Valves are like doors that open and close. They open to allow blood to flow through to the next chamber or to one of the arteries, and then they shut to keep blood from flowing backward.
When the heart's valves open and close, they make a "lub-DUB" sound that a doctor can hear using a stethoscope.
- The first sound-the "lub"-is made by the mitral and tricuspid valves closing at the beginning of systole (SIS-toe-lee). Systole is when the ventricles contract, or squeeze, and pump blood out of the heart.
- The second sound-the "DUB"-is made by the aortic and pulmonary valves closing at the beginning of diastole (di-AS-toe-lee). Diastole is when the ventricles relax and fill with blood pumped into them by the atria.
Arteries
The arteries are major blood vessels connected to your heart.
- The pulmonary artery carries blood pumped from the right side of the heart to the lungs to pick up a fresh supply of oxygen.
- The aorta is the main artery that carries oxygen-rich blood pumped from the left side of the heart out to the body.
- The coronary arteries are the other important arteries attached to the heart. They carry oxygen-rich blood from the aorta to the heart muscle, which must have its own blood supply to function.
Veins
The veins also are major blood vessels connected to your heart.
- The pulmonary veins carry oxygen-rich blood from the lungs to the left side of the heart so it can be pumped out to the body.
- The superior and inferior vena cavae are large veins that carry oxygen-poor blood from the body back to the heart.
For more information on how a healthy heart works, go to the Diseases and Conditions Index How the Heart Works article. This article contains animations that show how your heart pumps blood and how your heart's electrical system works.
Types of Holes in the Heart
Atrial Septal Defect
An atrial septal defect (ASD) is a hole in the part of the septum that separates the atria (the upper chambers of the heart). This hole allows oxygen-rich blood from the left atrium to flow into the right atrium instead of flowing into the left ventricle as it should.
This means that oxygen-rich blood gets pumped back to the lungs, where it has just been, instead of going to the body.
Cross-Section of a Normal Heart and a Heart With an Atrial Septal Defect
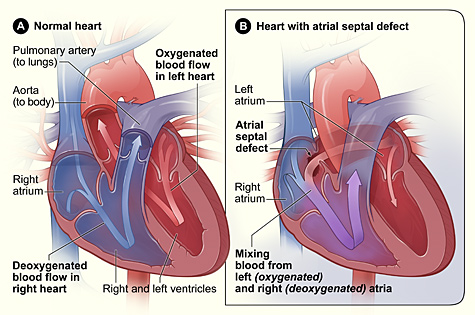
Figure A shows the normal structure and blood flow in the interior of the heart. Figure B shows a heart with an atrial septal defect. The hole allows oxygen-rich blood from the left atrium to mix with oxygen-poor blood from the right atrium.
An ASD can be small or large. Small ASDs allow only a little blood to flow from one atrium to the other. Small ASDs don't affect the way the heart works and don't need any special treatment. Many small ASDs close on their own as the heart grows during childhood.
Medium to large ASDs allow more blood to leak from one atrium to the other, and they're less likely to close on their own. Most children who have ASDs have no symptoms, even if they have large ASDs.
The three major types of ASDs are:
- Secundum. This defect is in the middle of the atrial septum. It's the most common form of ASD. About 8 out of every 10 babies born with ASDs have secundum defects. At least half of all secundum ASDs close on their own. However, this is less likely if the defect is large.
- Primum. This defect is in the lower part of the atrial septum. It often occurs along with problems in the heart valves that connect the upper and lower heart chambers. Primum defects aren't very common, and they don't close on their own.
- Sinus venosus. This defect is in the upper part of the atrial septum, near where a large vein (the superior vena cava) brings oxygen-poor blood from the upper body to the right atrium. Sinus venosus defects are rare, and they don't close on their own.
Atrial Septal Defect Complications
Over time, if an ASD isn't repaired, the extra blood flow to the right side of the heart and lungs may cause heart problems. Usually, most of these problems don't show up until adulthood, often around age 30 or later. Complications are rare in infants and children.
Possible complications include:
- Right heart failure. An ASD causes the right side of the heart to work harder because it has to pump extra blood to the lungs. Over time, the heart may become tired from this extra work and not pump well.
- Arrhythmias (ah-RITH-me-ahs). Extra blood flowing into the right atrium through an ASD can cause the atrium to stretch and enlarge. Over time, this can lead to arrhythmias (irregular heartbeats). Arrhythmia symptoms may include palpitations or a rapid heartbeat.
- Stroke. Usually, the lungs filter out small blood clots that can form on the right side of the heart. Sometimes a blood clot can pass from the right atrium to the left atrium through an ASD and be pumped out to the body. This type of clot can travel to an artery in the brain, block blood flow, and cause a stroke.
- Pulmonary hypertension (PH). PH is increased pressure in the pulmonary arteries. These arteries carry blood from your heart to your lungs to pick up oxygen. Over time, PH can damage the arteries and small blood vessels in the lungs. They become thick and stiff, making it harder for blood to flow through them.
These problems develop over many years and don't occur in children. They also are rare in adults because most ASDs either close on their own or are repaired in early childhood.
Ventricular Septal Defect
A ventricular septal defect (VSD) is a hole in the part of the septum that separates the ventricles (the lower chambers of the heart). The hole allows oxygen-rich blood to flow from the left ventricle into the right ventricle instead of flowing into the aorta and out to the body as it should.
Cross-Section of a Normal Heart and a Heart With a Ventricular Septal Defect
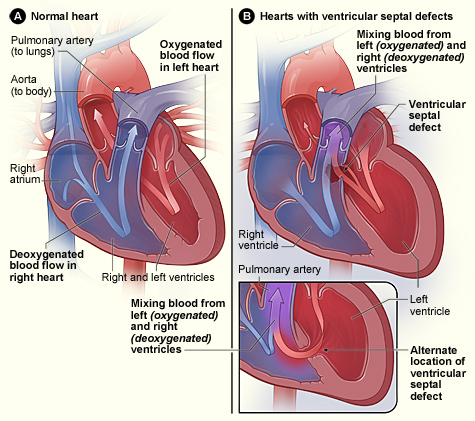
Figure A shows the normal structure and blood flow in the interior of the heart. Figure B shows two common locations for a ventricular septal defect. The defect allows oxygen-rich blood from the left ventricle to mix with oxygen-poor blood in the right ventricle.
An infant who is born with a VSD may have a single hole or more than one hole in the wall that separates the two ventricles. The defect also may occur by itself or with other congenital heart defects.
Doctors classify VSDs based on the:
- Size of the defect.
- Location of the defect.
- Number of defects.
- Presence or absence of a ventricular septal aneurysm-a thin flap of tissue on the septum. This tissue is harmless and can help a VSD close on its own.
VSDs can be small or large. Small VSDs don't cause problems and often may close on their own. Because small VSDs allow only a small amount of blood to flow between the ventricles, they're sometimes called restrictive VSDs. Small VSDs don't cause any symptoms.
Medium VSDs are less likely to close on their own. They may require surgery to close and may cause symptoms during infancy and childhood.
Large VSDs allow a large amount of blood to flow from the left ventricle to the right ventricle. They're sometimes called nonrestrictive VSDs. A large VSD is less likely to close completely on its own, but it may get smaller over time. Large VSDs often cause symptoms in infants and children, and surgery usually is needed to close them.
VSDs are found in different parts of the septum.
- Membranous VSDs are located near the heart valves. These VSDs can close at any time.
- Muscular VSDs are found in the lower part of the septum. They're surrounded by muscle, and most close on their own during early childhood.
- Inlet VSDs are located close to where blood enters the ventricles. They're less common than membranous and muscular VSDs.
- Outlet VSDs are found in the part of the ventricle where blood leaves the heart. These are the rarest type of VSD.
Ventricular Septal Defect Complications
Over time, if a VSD isn't repaired, it may cause heart problems. A moderate to large VSD can cause:
- Heart failure. Infants who have large VSDs may develop heart failure because the left side of the heart pumps blood into the right ventricle in addition to its normal work of pumping blood to the body. The increased workload on the heart also increases the heart rate and the body's demand for energy.
- Growth failure, especially in infancy. A baby may not be able to eat enough to keep up with his or her body's increased energy demands. As a result, the baby may lose weight or not grow and develop normally.
- Arrhythmias (irregular heartbeats). The extra blood flowing through the heart can cause areas of the heart to stretch and enlarge. This can disturb the heart's normal electrical activity, leading to arrhythmias.
- PH. The high pressure and high volume of extra blood pumped through a large VSD into the right ventricle and lungs can scar the lung's delicate arteries. Today, PH rarely develops because most large VSDs are repaired in infancy.
What Causes Holes in the Heart?
Mothers of children who are born with atrial septal defects (ASDs), ventricular septal defects (VSDs), or other types of heart defects often think that they did something wrong during the pregnancy to cause the problems. However, most of the time, doctors don't know why congenital heart defects develop.
Heredity may play a role in some heart defects. For example, a parent who has a congenital heart defect is slightly more likely than other people to have a child with the problem. Very rarely, more than one child in a family is born with a heart defect.
Children who have genetic disorders, such as Down syndrome, often have congenital heart defects. Half of all babies who have Down syndrome have congenital heart defects.
Smoking during pregnancy also has been linked to several congenital heart defects, including septal defects.
Scientists continue to search for the causes of congenital heart defects.
What Are the Signs and Symptoms of Holes in the Heart?
Atrial Septal Defect
Many babies who are born with atrial septal defects (ASDs) have no signs or symptoms. When signs and symptoms do occur, heart murmur is the most common. A heart murmur is an extra or unusual sound heard during a heartbeat.
Often, a heart murmur is the only sign of an ASD. However, not all murmurs are signs of congenital heart defects. Many healthy children have heart murmurs. Doctors can listen to heart murmurs and tell whether they're harmless or signs of heart problems.
Over time, if a large ASD isn't repaired, the extra blood flow to the right side of the heart can damage the heart and lungs and cause heart failure. This doesn't occur until adulthood. Signs and symptoms of heart failure include:
- Fatigue (tiredness)
- Tiring easily during physical activity
- Shortness of breath
- A buildup of blood and fluid in the lungs
- A buildup of fluid in the feet, ankles, and legs
Ventricular Septal Defect
A heart murmur usually is present in ventricular septal defect (VSD), and it may be the first and only sign of this defect. Heart murmurs often are present right after birth in many infants. However, the murmurs may not be heard until the babies are 6 to 8 weeks old.
Most newborns who have VSDs don't have heart-related symptoms. However, babies who have medium or large VSDs can develop heart failure. Signs and symptoms of heart failure usually occur during the baby's first 2 months of life.
The signs and symptoms of heart failure from VSD are similar to those listed above for ASD, but they occur in infancy.
A major sign of heart failure in infancy is difficulty feeding and poor growth. VSD signs and symptoms are rare after infancy because the defect either decreases in size on its own or is repaired.
How Are Holes in the Heart Diagnosed?
Doctors usually diagnose holes in the heart based on results from a physical exam and tests and procedures. The exam findings for an atrial septal defect (ASD) often aren't obvious, so the diagnosis sometimes isn't made until later childhood or even adulthood.
Ventricular septal defects (VSDs) have a very distinct heart murmur, so a diagnosis usually is made in infancy.
Specialists Involved
Doctors who specialize in diagnosing and treating heart problems are called cardiologists. Pediatric cardiologists take care of babies and children who have heart problems. Cardiac surgeons repair heart defects using surgery.
Physical Exam
During a physical exam, your child's doctor will listen to your child's heart and lungs with a stethoscope. The doctor also will look for signs of a heart defect, such as a heart murmur or signs of heart failure.
Diagnostic Tests and Procedures
Your child's doctor may recommend several tests to diagnose an ASD or VSD. These tests also will help the doctor determine the location and size of the defect.
Echocardiography
Echocardiography (echo) is a painless test that uses sound waves to create a moving picture of the heart. During the test, the sound waves (called ultrasound) bounce off the structures of the heart. A computer converts the sound waves into pictures on a screen.
Echo allows the doctor to clearly see any problem with the way the heart is formed or the way it's working.
Echo is an important test for both diagnosing a hole in the heart and following the problem over time. Echo can show problems with the heart's structure and how the heart is reacting to the problems. Echo will help your child's cardiologist decide whether and when treatment is needed.
EKG
An EKG is a simple, painless test that records the heart's electrical activity. The test shows how fast the heart is beating and its rhythm (steady or irregular). It also records the strength and timing of electrical signals as they pass through each part of the heart.
An EKG can detect whether one of the heart's chambers is enlarged, which can help diagnose a heart problem.
Chest X Ray
A chest x ray is a painless test that creates pictures of the structures in the chest, such as the heart and lungs. This test can show whether the heart is enlarged or whether the lungs have extra blood flow or extra fluid, a sign of heart failure.
Pulse Oximetry
Pulse oximetry shows how much oxygen is in the blood. For this test, a small sensor is attached to a finger or toe (like an adhesive bandage). The sensor gives an estimate of how much oxygen is in the blood.
Cardiac Catheterization
During cardiac catheterization (KATH-e-ter-i-ZA-shun), a thin, flexible tube called a catheter is put into a vein in the arm, groin (upper thigh), or neck and threaded to the heart.
Special dye is injected through the catheter into a blood vessel or a chamber of the heart. The dye allows the doctor to see the flow of blood through the heart and blood vessels on an x-ray image.
The doctor also can use cardiac catheterization to measure the pressure inside the heart chambers and blood vessels. This can help the doctor determine whether blood is mixing between the two sides of the heart.
Cardiac catheterization also is used to repair some heart defects. For more information, go to "How Are Holes in the Heart Treated?"
How Are Holes in the Heart Treated?
Many holes in the heart don't need treatment, but some do. Most holes in the heart that need treatment are repaired in infancy or early childhood. Sometimes, adults are treated for holes in the heart if problems develop.
The treatment your child receives depends on the type, location, and size of the hole. Other factors include your child's age, size, and general health.
Treating Atrial Septal Defect
Periodic checkups are done to see whether an atrial septal defect (ASD) closes on its own. About half of all ASDs close on their own over time, and about 20 percent close within the first year of life.
Your child's doctor will let you know how often your child should have checkups. For an ASD, frequent checkups aren't needed.
When treatment of an ASD is required, it involves catheter or surgical procedures to close the hole. Doctors often decide to close an ASD in children who still have medium to large holes by the time they're 2 to 5 years old.
Catheter Procedure
Until the early 1990s, surgery was the usual method for closing all ASDs. Now, thanks to medical advances, doctors can use catheter procedures to close secundum ASDs, the most common type of ASD. For this procedure, your child is given medicine so he or she will sleep through it and not feel any pain.
During the procedure, the doctor inserts a catheter (a thin, flexible tube) into a vein in the groin (upper thigh) and threads it to the heart's septum. The catheter has a tiny umbrella-like device folded up inside it.
When the catheter reaches the septum, the device is pushed out of the catheter and positioned so that it plugs the hole between the atria. The device is secured in place and the catheter is withdrawn from the body.
Within 6 months, normal tissue grows in and over the device. There is no need to replace the closure device as the child grows.
Doctors often use echocardiography (echo) or transesophageal (tranz-ih-sof-uh-JEE-ul) echo (TEE) as well as angiography (an-jee-OG-ra-fee) to guide them in threading the catheter to the heart and closing the defect. TEE is a special type of echo that takes pictures of the heart through the esophagus (the passage leading from the mouth to the stomach).
Catheter procedures are much easier on patients than surgery because they involve only a needle puncture in the skin where the catheter is inserted. This means that recovery is faster and easier.
The outlook for children having this procedure is excellent. Closures are successful in more than 9 out of 10 patients, with no significant leakage. Rarely, a defect is too large for catheter closure and surgery is needed.
Surgery
Open-heart surgery generally is done to repair primum or sinus venosus ASDs. Your child is given medicine so that he or she will sleep through the surgery and not feel any pain.
During the surgery, the cardiac surgeon makes an incision (cut) in the chest to reach the ASD. He or she then repairs the defect with a special patch that covers the hole. Your child is placed on a heart-lung bypass machine so that the heart can be opened to do the surgery.
The outlook for children after ASD surgery is excellent. On average, children spend 3 to 4 days in the hospital before going home. Complications, such as bleeding and infection, from ASD surgery are very rare.
Some children may develop inflammation of the outer lining of the heart, a condition called pericarditis (PER-i-kar-DI-tis). This causes fluid to collect around the heart in the weeks after surgery. This complication of heart surgery usually resolves with medicine.
While in the hospital, your child will be given medicines as needed to reduce pain or anxiety. The doctors and nurses at the hospital will teach you how to care for your child at home.
They will talk about preventing blows to the chest as the incision heals, limiting activity while your child recovers, bathing, scheduling followup medical appointments, and determining when your child can go back to his or her regular activities.
Treating Ventricular Septal Defect
Doctors may choose to monitor and observe children who have ventricular septal defects (VSDs) but don't have symptoms of heart failure. This means regular checkups and tests to see whether the defect closes on its own or gets smaller.
More than half of VSDs eventually close, usually by the time a child is in preschool. Your child's doctor will let you know how often your child should be checked. Checkups may range from once a month to once every 1 or 2 years.
When treatment for a VSD is required, options include extra nutrition and surgery to close the VSD.
The doctor may recommend surgery if your child's VSD:
- Is large
- Is causing symptoms
- Is medium-sized and is causing enlarged heart chambers
- Affects the aortic valve
Extra Nutrition
Some infants who have VSDs don't grow and develop or gain weight as they should. These infants usually:
- Have large VSDs
- Are born prematurely
- Tire easily during feeding
Doctors usually recommend extra nutrition or special feedings for these infants. These feedings are high-calorie formulas or breast milk supplements that give babies extra nourishment.
In some cases, tube feeding is needed. Food is given through a small tube that's placed through the nose and into the stomach. Tube feeding can add to or take the place of bottle feeding. This treatment usually is temporary because a VSD that causes symptoms will likely need surgery.
Surgery
Most doctors recommend surgery to close large VSDs that are causing symptoms or haven't closed by the time children are 1 year old. Surgery may be needed earlier if:
- The child fails to gain weight
- Medicines are needed to control the symptoms of heart failure
Rarely, medium-sized VSDs that are causing enlarged heart chambers are treated with surgery after infancy. However, most VSDs that need surgery are repaired in the first year of life.
Living With Holes in the Heart
The outlook for children who have atrial septal defects (ASDs) or ventricular septal defects (VSDs) is excellent. Advances in treatment allow most children who have these heart defects to live normal, active, and productive lives with no decrease in lifespan.
Many children who have these defects need no special care or only occasional checkups with a cardiologist (a heart specialist) as they go through life.
Living With an Atrial Septal Defect
Small ASDs often close on their own and don't cause complications or require treatment. Children and adults who have small ASDs that don't close and don't cause symptoms are healthy and don't need treatment.
Many others who have ASDs that don't close have catheter procedures or surgery to close the holes and prevent possible long-term complications. Children recover well from these procedures and lead normal, healthy lives. Adults also do well after closure procedures.
Ongoing Care
Arrhythmias. The risk of arrhythmias (irregular heartbeats) increases before and after surgery. Adults who have ASDs and are older than 40 are especially likely to have arrhythmias. People who had arrhythmias before surgery are more likely to have them after surgery.
Followup care. Regular followup care into adult life is advised for people who have had:
- An ASD repaired as an adult
- Arrhythmias before and after surgery
- An ASD repaired with a catheter procedure
- Pulmonary hypertension (increased pressure in the pulmonary arteries) at the time of surgery
Antibiotics. Children who have severe heart defects may be at slightly increased risk for infective endocarditis (IE). IE is a serious infection of the inner lining of your heart chambers and valves.
ASDs aren't associated with a risk of IE, except in the 6 months after repair (for both catheter procedures and surgery).
In a few situations, your child's doctor or dentist may give your child antibiotics before medical or dental procedures (such as surgery or dental cleanings) that could allow bacteria into the bloodstream. Your child's doctor will tell you whether your child needs to take antibiotics before such procedures.
To reduce the risk of IE, gently brush your young child's teeth every day as soon as they begin to come in. As your child gets older, make sure he or she brushes every day and sees a dentist regularly. Talk with your child's doctor and dentist about how to keep your child's mouth and teeth healthy.
Special Considerations for Children and Teens
- Activity. Children who have a repaired or closed ASD have no restrictions on their activity.
- Growth and development. Children who have ASDs don't have growth or development problems.
- Regular health care. Your child should see his or her regular doctor for routine health care.
- Additional surgery or procedures. When a child has an ASD, but no other heart defects, additional surgery isn't needed.
Special Considerations for Adults
When an adult has an ASD repaired, his or her cardiologist or surgeon will explain what to expect during the recovery period and when to return to driving, working, exercising, and other activities.
Living With a Ventricular Septal Defect
Children who have small VSDs have no symptoms and only need occasional followup with a cardiologist.
Children and adults who've had successful repair of VSDs and have no other congenital heart defects can expect to lead normal, healthy, and active lives.
Ongoing Care
Sometimes problems and risks remain after surgical closure. They include:
- Arrhythmias. Serious and frequent arrhythmias require regular medical followup. The risk of arrhythmia is greater if surgery is done later in life.
- Residual or remaining VSD. This usually is due to a leak at the edge of the patch used to close the hole. These VSDs tend to be very small and don't cause problems. They very rarely require another operation.
Antibiotics. Children who have severe heart defects may be at slightly increased risk for IE, a serious infection of the inner lining of your heart chambers and valves.
In a few situations, your child's doctor or dentist may give your child antibiotics before medical or dental procedures (such as surgery or dental cleanings) that could allow bacteria into the bloodstream. Your child's doctor will tell you whether your child needs to take antibiotics before such procedures.
To reduce the risk of IE, gently brush your young child's teeth every day as soon as they begin to come in. As your child gets older, make sure he or she brushes every day and sees a dentist regularly. Talk with your child's doctor and dentist about how to keep your child's mouth and teeth healthy.
Special Considerations for Children and Teens
- Activity. Children who have small VSDs that don't require surgery or who have recovered from VSD repair shouldn't have activity restrictions. Be sure to check with your child's doctor about whether your child can take part in sports.
- Growth and development. Your pediatrician or family doctor will check your child's growth and development at each routine checkup. Babies who have large VSDs may not grow as quickly as other infants. These babies usually catch up after their VSDs are closed.
- Regular health care. Your child should see his or her regular doctor for routine health care.
- Additional surgery or procedures. Teens and young adults rarely need additional surgeries once VSDs are closed or repaired.








