Lung Transplant
A lung transplant is surgery to remove a person's diseased lung and replace it with a healthy lung from a deceased donor.
Lung transplants are used for people who are likely to die from lung disease within 1 to 2 years. Their conditions are so severe that other treatments, such as medicines or breathing devices, no longer work.
Overview
Lung transplants aren't very common because of the small number of donor organs available. About 1,800 lung transplants were done in the United States in 2010. More donor lungs would mean a larger number of suitable lungs available for transplant.
Most people who have lung transplants are between the ages of 18 and 65. The surgery sometimes is used for children and older adults. This article focuses on lung transplants in adults.
Each patient must go through a careful screening process to make sure he or she is a good candidate for a lung transplant. Donor lungs also are carefully screened to make sure they're healthy enough to be used for a transplant.
The Organ Procurement and Transplantation Network (OPTN) manages the nationwide organ-sharing process. OPTN also maintains the waiting lists for all organ donations.
The number of people on the lung transplant waiting list changes often. About half of the people on the list receive a lung in any given year.
Some people get one lung during a transplant. This is called a single-lung transplant. Other people get two lungs, which is called a double-lung transplant. The number of double-lung transplants has gone up over the years. More double-lung transplants are done now than single-lung transplants.
Some people who have severe heart disease and lung disease get a heart and lung(s). This is called a heart–lung transplant.
A rare kind of lung transplant is a living donor lobar lung transplant. For this surgery, a healthy adult donates a segment, or lobe, of one lung to another person. This type of transplant usually is done in children.
Outlook
Lung transplants are a "last resort" treatment for people who have severe disease and no other medical options.
A lung transplant can improve a person's quality of life. For people who have certain lung problems, a transplant also may help them live longer than they would without the surgery.
Lung transplants have serious risks. Your body may reject the new lung, or you may get infections. The short- and long-term complications of a lung transplant can be life threatening.
Other Names for Lung Transplant
- Double-lung transplant
- Living donor lobar lung transplant
- Single-lung transplant
Who Needs a Lung Transplant?
Your doctor may recommend a lung transplant if you have severe lung disease that's getting worse. If your condition is so serious that other treatments don't work, a lung transplant may be the only option.
Lung transplants most often are used to treat people who have severe:
- COPD (chronic obstructive pulmonary disease). COPD is the most common reason why adults need lung transplants. COPD is a progressive disease that makes it hard to breathe. “Progressive” means the disease gets worse over time.
- Idiopathic pulmonary fibrosis (IPF). IPF is a condition in which tissue deep in your lungs becomes thick and stiff, or scarred, over time.
- Cystic fibrosis (CF). CF is the most common reason in children for needing a lung transplant. CF is an inherited disease that causes thick, sticky mucus to build up in the lungs. This leads to repeated, serious lung infections.
- Alpha-1 antitrypsin deficiency (AAT deficiency). AAT deficiency is a condition that raises your risk for certain types of lung disease, especially if you smoke.
- Pulmonary hypertension (PH). PH is increased pressure in the pulmonary arteries. These arteries carry blood from your heart to your lungs to pick up oxygen.
Applying to a Lung Transplant Program
Lung transplants are done in medical centers (large hospitals) where the staff has a lot of organ transplant experience. If you need a lung transplant, you must apply to a center's transplant program.
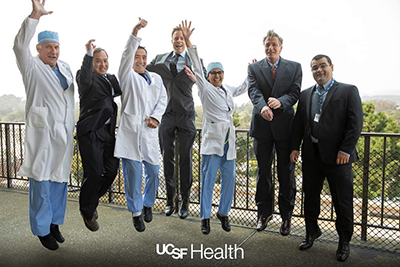
Transplant teams at the medical center manage all parts of the center's transplant program. Transplant team members may include a:
- Thoracic (THOR-as-ik) surgeon. This is a doctor who does lung and chest surgeries.
- Pulmonologist. This is a doctor who specializes in lung diseases and conditions.
- Cardiologist. This is a doctor who specializes in heart diseases and conditions.
- Immunologist. This is a doctor who specializes in immune system disorders.
- Respiratory (RES-pi-rah-tor-e) technician. This is a person who cares for people who have breathing and lung problems.
- Transplant coordinator. This is a person who arranges the surgery.
Other team members may include a social worker, psychiatrist, financial coordinator, and other specialists and medical personnel, such as a nutritionist and nurses.
The transplant team will need to find out whether you're a candidate for a lung transplant. They will want to make sure you're healthy enough to have the surgery and go through a recovery program.
To do this, they will ask about your medical history. The team will want to know whether you have other serious illnesses or conditions, such as cancer, HIV, or hepatitis. They also will ask whether you've had a major chest surgery. A previous chest surgery may make it hard to do a lung transplant.
The team also will want to know whether you smoke or use alcohol or drugs.
You also will have tests to show whether you're healthy enough for a lung transplant. Tests may include:
- Lung function tests. These tests measure how much air you can breathe in and out, how fast you can breathe air out, and how well your lungs deliver oxygen to your blood.
- Blood tests. Blood tests help doctors check for certain diseases and conditions. They also help check the function of your organs and show how well treatments are working.
- Chest CT scan. This test creates precise pictures of the structures inside your chest, such as your lungs.
- EKG (electrocardiogram). This test detects and records the heart's electrical activity.
- Echocardiography (echo). Echo uses sound waves to create pictures of your heart.
- Right cardiac catheterization. This test measures blood pressure in the right side of your heart. The results give clues about heart valve disease, heart failure, or lung problems.
You'll talk with team members to make sure you're mentally and emotionally willing to accept the risks of the transplant process and later treatment. The team may ask whether you have a good support network of family and friends.
What To Expect Before a Lung Transplant
If you get into a medical center's transplant program, you'll be placed on the Organ Procurement and Transplantation Network's (OPTN's) national waiting list. Your transplant team will work with you to make sure you're ready for the transplant if a donor lung becomes available.
Waiting for a donor lung can be frustrating. However, you can do several things to prepare.
- Go to all of your medical appointments with the transplant team. Take all of your medicines as prescribed.
- Stay as healthy as possible. Don't smoke, and follow your doctor's advice about breathing exercises, physical activity, diet, and drinking alcohol.
- Talk regularly with your transplant team. You and your family should know what to do if a donor lung becomes available. You also should know what to expect before, during, and after the transplant.
- Be ready to go to the transplant center right away if a donor lung becomes available. Make sure the transplant center knows how to reach you at any time, day or night. Your transplant team may give you a pager so they can reach you right away. Make travel and lodging plans in advance. Have a packed suitcase ready to go.
While you wait for a lung, you may feel worried, scared, anxious, or depressed. These feelings are normal in this situation. Talk with your health care team about how you feel. They can offer tips for coping with your emotions. Family and friends also can offer support.
When a Donor Lung Becomes Available
OPTN matches donor lungs to recipients based on need. OPTN will consider how severe a person's disease is and how quickly it's worsening. OPTN also will consider whether the transplant will improve the recipient's chances of survival, and by how much.
Organs are matched for blood type and the size of the donor lung and the recipient.
If OPTN and your transplant center think they have a good match for you, the center will ask you to come in as soon as possible.
Once you arrive, your team will do tests to make sure you're healthy enough to have the surgery and that the lung is a good match. If you're healthy enough and the lung is a good match, the team will prepare you for surgery.
What To Expect During a Lung Transplant
Just before lung transplant surgery, you will get general anesthesia (AN-es-THE-ze-ah). The term "anesthesia" refers to a loss of feeling and awareness. With general anesthesia, you will be asleep during the surgery and not feel any pain.
Once you're asleep, your doctors will make a small incision (cut) in your chest. Next, they will insert a central venous catheter into a vein. This tube allows easy access to your bloodstream. Doctors use it to deliver fluids and medicines to your body.
Your doctors also will insert a tube in your mouth and down your windpipe to help you breathe. They also will insert a tube in your nose and down to your stomach to drain contents from your stomach. A catheter will be used to keep your bladder empty.
The surgeon will make a cut in your chest to open it. He or she will then cut the main airway to your diseased lung and the blood vessels connecting your lung to your heart.
The surgeon will remove your diseased lung and place the donor organ in your chest. Then the surgeon will connect the main airway of the donor lung to your airway and its blood vessels to your heart.
Lung Transplant
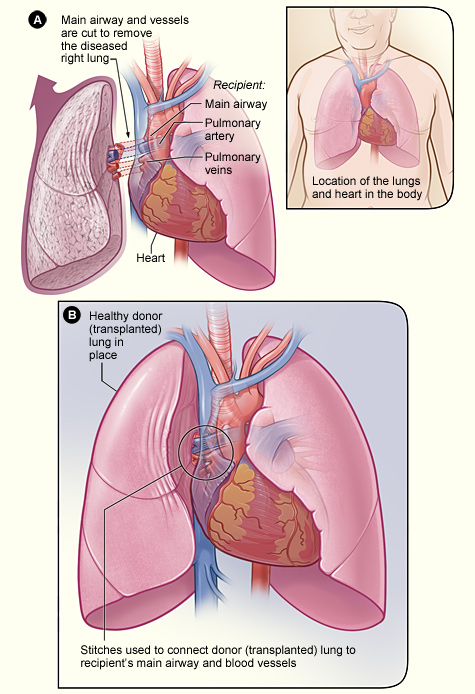
The illustration shows the process of a lung transplant. In figure A, the airway and blood vessels between a recipient’s diseased right lung and heart are cut. The inset image shows the location of the lungs and heart in the body. In figure B, a healthy donor lung is stitched to the recipient’s blood vessels and airway.
If you're having a double-lung transplant, you may be connected to a heart-lung bypass machine. This machine takes over for your heart and pumps oxygen-rich blood to your body. For more information about the heart-lung bypass machine and an illustration, go to the Diseases and Conditions Index Heart Surgery article.
During a double-lung transplant, the surgeon will remove your diseased lungs, one at a time, and replace them with the donor lungs.
A single-lung transplant usually takes 4 to 8 hours. A double-lung transplant usually takes 6 to 12 hours.
Some people may need a heart–lung transplant. A heart–lung transplant is surgery in which both the heart and lung(s) are replaced with healthy organs from a deceased donor. For this surgery, you're connected to a heart-lung bypass machine.
What To Expect After a Lung Transplant
Recovery in the Hospital
After lung transplant surgery, you'll go to the hospital's intensive care unit (ICU) for at least several days. The tubes that were inserted before surgery will remain for a few days.
The tube in your windpipe helps you breathe. Other tubes deliver medicines to, and drain fluids from, your body. You also will have sticky patches called electrodes attached to your chest to monitor your heart.
After leaving the ICU, you'll go to a hospital room. The staff will carefully oversee your recovery.
You'll be taught how to do deep breathing exercises with an incentive spirometer (spi-ROM-eh-ter). This hand-held device helps you take slow, deep breaths. You also may have lung function tests that use a regular spirometer. This device measures how much air your lungs can hold. It also measures how fast you can blow air out of your lungs after taking a deep breath.
You'll need to cough often. Coughing helps clear fluids from your lungs so they can work well. A nurse will show you how to hold a pillow tightly near your incision site while you cough to help decrease discomfort.
Your immune system will regard your new lung as a "foreign object." It will create antibodies (proteins) against the lung. This may cause your body to reject the new organ. To prevent this, your doctor will prescribe medicines to suppress your immune system.
Because these medicines can weaken your immune system, you're more likely to get an infection after the transplant. Your medical team will take steps to prevent infections while you're in the hospital.
On average, people who have a lung transplant stay in the hospital from 1 to 3 weeks. However, some people have complications and stay much longer.
Recovery After Leaving the Hospital
Before you leave the hospital, your medical team will teach you how to keep track of your overall health. You'll learn how to watch your weight and check your blood pressure, pulse, and temperature. Staff also will show you how to check your lung function.
You'll also learn the signs of the two main complications of lung transplant surgery: rejection and infection. (For more information, go to "What Are the Risks of Lung Transplant?")
For the first 3 months after surgery, you'll go to the hospital often for blood tests, chest x rays, lung function tests, and other tests. After 3 months, if you're doing well, you'll visit less often.
Making healthy lifestyle choices is very important. Not smoking, following a healthy diet, and following your doctor's advice on using alcohol will help you recover and stay as healthy as possible.
A healthy diet includes a variety of fruits, vegetables, and whole grains. It also includes lean meats, poultry, fish, beans, and fat-free or low-fat milk or milk products. A healthy diet is low in saturated fat, trans fat, cholesterol, sodium (salt), and added sugar.
For more information about following a healthy diet, go to the National Heart, Lung, and Blood Institute's Aim for a Healthy WeightWeb site, "Your Guide to a Healthy Heart," and "Your Guide to Lowering Your Blood Pressure With DASH." All of these resources include general information about healthy eating.
Your doctor may recommend pulmonary rehabilitation (PR) after your lung transplant surgery. PR is a broad program that may include exercise training, education, counseling, and more. For more information, go to the Health Topics Pulmonary Rehabilitationarticle.
Emotional Issues and Support
Having a lung transplant may cause fear, anxiety, and stress. While you're waiting for a lung transplant, you may worry that you won't live long enough to get a new lung. After surgery, you may feel overwhelmed, depressed, or worried about complications.
All of these feelings are normal for someone going through major surgery. Talk about how you feel with your health care team. Talking to a professional counselor also can help. If you’re very depressed, your doctor may recommend medicines or other treatments that can improve your quality of life.
Support from family and friends also can help relieve stress and anxiety. Let your loved ones know how you feel and what they can do to help you.
What Are the Risks of Lung Transplant?
A lung transplant can improve your quality of life and extend your lifespan. The first year after the transplant is the most critical. This is when the risk of complications is highest.
In recent years, short-term survival after lung transplant has improved. Recent data on single-lung transplants show that:
- About 78 percent of patients survive the first year
- About 63 percent of patients survive 3 years
- About 51 percent of patients survive 5 years
Survival rates for double-lung transplants are slightly better. Recent data show that the median survival for single-lung recipients is 4.6 years. The median survival for double-lung recipients is 6.6 years. Talk with your doctor about what these figures may mean for you.
Complications
The major complications of lung transplant are rejection and infection.
Rejection
Your immune system will regard your new lung as a "foreign object." It will create antibodies (proteins) against the lung. This may cause your body to reject the new organ.
To prevent this, your doctor will prescribe medicines to suppress your immune system. You’ll need to take these medicines for the rest of your life.
Rejection is most common in the first 6 months after surgery, but it can happen any time after the transplant. Rejection can happen slowly or suddenly. Your doctor will teach you how to spot possible signs and symptoms of rejection. If you know these signs and symptoms, you can seek treatment right away.
Signs and symptoms of rejection include:
- Fever and flu-like symptoms
- Chest congestion
- Coughing
- Shortness of breath
- New pain around the lung
- Generally feeling unwell
If you have any of these signs or symptoms, seek medical care. Your doctor may prescribe medicines to treat the rejection and prevent complications.
These medicines may cause side effects, such as headaches, nausea (feeling sick to your stomach), and flu-like symptoms. If you have side effects, tell your doctor. He or she may change your medicines or adjust the doses.
Infection
The medicines you take to prevent the rejection of your new lung may weaken your immune system. As a result, you're more likely to get infections.
While you're in the hospital, staff will take special steps to prevent you from getting infections. After you leave the hospital, you also can take steps to prevent infections:
- Wash your hands often.
- Take care of your teeth and gums.
- Protect your skin from scratches and sores.
- Stay away from crowds and from people who have colds and the flu.
Other Risks
Long-term use of medicines that suppress the immune system can cause diabetes, kidney damage, and osteoporosis (thinning of the bones). These medicines also can increase the risk of cancer. Talk with your doctor about the long-term risks of using these medicines.
Clinical Trials
The National Heart, Lung, and Blood Institute (NHLBI) is strongly committed to supporting research aimed at preventing and treating heart, lung, and blood diseases and conditions and sleep disorders.
NHLBI-supported research has led to many advances in medical knowledge and care. Often, these advances depend on the willingness of volunteers to take part in clinical trials.
Clinical trials test new ways to prevent, diagnose, or treat various diseases and conditions. For example, new treatments for a disease or condition (such as medicines, medical devices, surgeries, or procedures) are tested in volunteers who have the illness. Testing shows whether a treatment is safe and effective in humans before it is made available for widespread use.
By taking part in a clinical trial, you can gain access to new treatments before they’re widely available. You also will have the support of a team of health care providers, who will likely monitor your health closely. Even if you don’t directly benefit from the results of a clinical trial, the information gathered can help others and add to scientific knowledge.
If you volunteer for a clinical trial, the research will be explained to you in detail. You’ll learn about treatments and tests you may receive, and the benefits and risks they may pose. You’ll also be given a chance to ask questions about the research. This process is called informed consent.
If you agree to take part in the trial, you’ll be asked to sign an informed consent form. This form is not a contract. You have the right to withdraw from a study at any time, for any reason. Also, you have the right to learn about new risks or findings that emerge during the trial.
For more information about clinical trials related to lung diseases or lung transplants, talk with your doctor. You also can visit the following Web sites to learn more about clinical research and to search for clinical trials:
- http://clinicalresearch.nih.gov
- www.clinicaltrials.gov
- www.nhlbi.nih.gov/studies/index.htm
- www.researchmatch.org
Links to Other Information About Lung Transplant
Non-NHLBI Resources
- Lung Transplantation (MedlinePlus)
Clinical Trials
- Clinical Trials (Health Topics)
- Current Research (ClinicalTrials.gov)
- NHLBI Clinical Trials
- NHLBI Pediatric Clinical Trials
- NIH and Clinical Research (National Institutes of Health)
- ResearchMatch(link is external) (funded by the National Institutes of Health)