Minimally Invasive Mitral Valve Surgery
|
|
The mitral valve consists of two leaflets, supported by chordae and papillary muscles, and located between the left atrium and left ventricle of the heart. The mitral valve prevents blood from leaking back into the lungs when the heart contracts. When the valve fails, patients may be severely affected.
Degenerative mitral valve disease is a common disorder affecting around 2% of the population. Common findings include a “prolapse” ( slipping or falling our of place), due to elongation or rupture of the chordal apparatus. When the two leaflets fail to close tightly, the mitral valve becomes insufficient, sometimes allowing blood to leak back into the atrium from the ventricle.
A prolapse can occur on either the anterior (front) leaflet or the posterior (rear) leaflet. Usually, the annulus, where the leaflets attach, is also dilated or enlarged.
 |
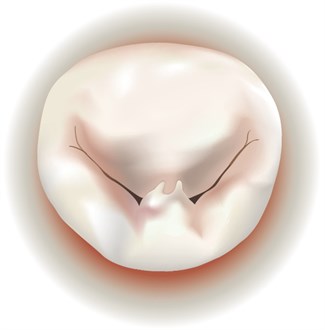 |
| Mitral Valve Prolapse on Anterior Leaflet | Mitral Valve Prolapse on Posterior Leaflet |
Why is Mitral Valve Insufficiency Dangerous?
Patients may become symptomatic, experiencing shortness of breath, reduced stamina, fatigue during exercise (exercise intolerance), and arrhythmia (irregular heartbeat). Moreover, severe mitral insufficiency reduces life expectancy, even in patients who are asymptomatic.
When Should Mitral Valve Insufficiency Be Treated?
Large studies have demonstrated that severe mitral valve insufficiency should be repaired early on before irreversible structural changes in the heart occur, a treatment strategy also recommended by both the American Heart Association and European Society of Cardiology. Unless treated before the heart structurally remodels, patients will experience reduced life expectancy (as compared with healthy patients without evidence of heart disease).
Can Surgery Be Performed Using Keyhole Incisions?
Patients with isolated mitral valve disease may be candidates for minimally invasive surgery, so long as they do not have clinically relevant aortic valve disease or coronary artery disease. Surgeons perform the operation by making only a small 4-6 cm incision on the right side of the chest instead of the large midline-incision and division of the sternum used traditional open surgery.
 |
| Small, 4-6 cm Incision on the Right Side of The Chest |
The surgery is performed through the small space between the ribs. The heart-lung machine is inserted via a small incision in the groin, allowing the heart to be stopped during repair of the valve. A soft retractor is inserted, which gently opens the narrow space between the ribs, enabling the surgeon to insert the specialized minimally invasive instruments. An endoscope, ideally with a 3D camera, is inserted that will provide a high-resolution image of the mitral valve.
Using this technique, the stability of the chest is fully preserved, patients recover more quickly, and the minimal scar will be barely visible after the patient recovers.
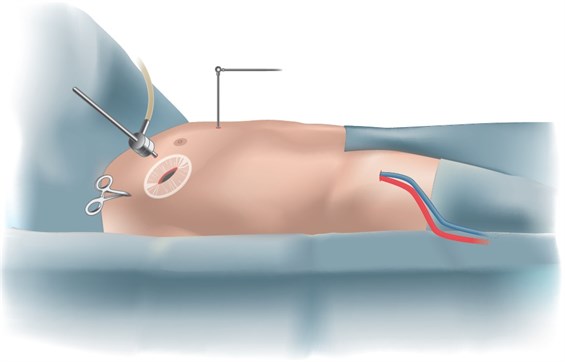 |
| Surgical Setup for Minimally Invasive Mitral Valve Surgery |
What are the Surgical Options?
The preferred surgical strategy for treatment of mitral valve disease is to repair the patient's own mitral valve (vs.replacing it). The advantages of repair include:
- Prolonged durability of the repaired valve
- Prolonged life expectancy
- Avoidance of long-term anticoagulation
- Better preservation of heart function
This is especially true when techniques are used to preserve the maximum amount of native mitral valve tissue, and where artificial chordae are used to correct the valve geometry. The results have proven to be long lasting and durable.
Only mitral valves showing extensive calcification or active bacterial infection may, under certain circumstances, need outright replacement .
What Happens During Surgery to Repair the Mitral Valve?
During the operation, the valve is thoroughly inspected and a strategy developed for performing the repair. In the example below, several chords to the anterior leaflet are ruptured as well as leaflet prolapse and annulus dilatation.
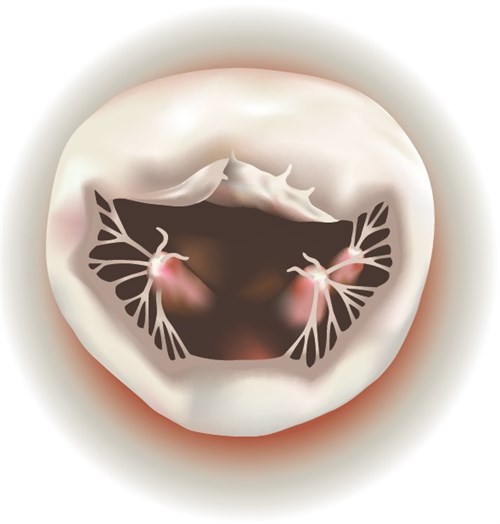 |
| Chords to the Anterior Leaflet Ruptured with Leaflet Prolapse and Annulus Dilatation |
Artificial chords made out of GoreTex, which function like natural chords, are inserted at the location of the ruptured chords,. The sutures are then passed through the papillary muscles and are extended to the free edge of the leaflet.
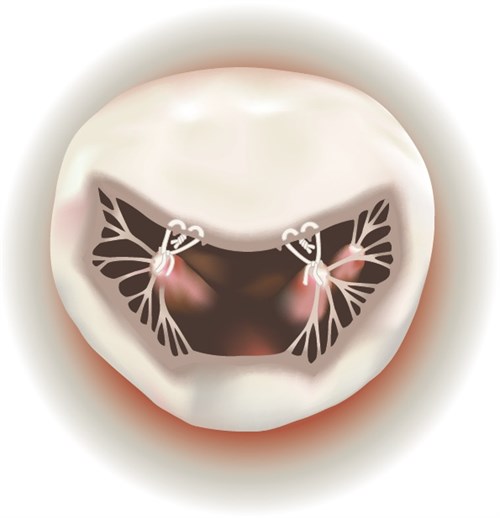 |
| Artificial Goretex Chords Inserted and Sutures Passed through Papillary Muscles |
The suture length is then adjusted to conform to the geometry of the valve. Later, an annuloplasty ring is sized and implanted to support the repair, and maintain the optimized valve geometry.
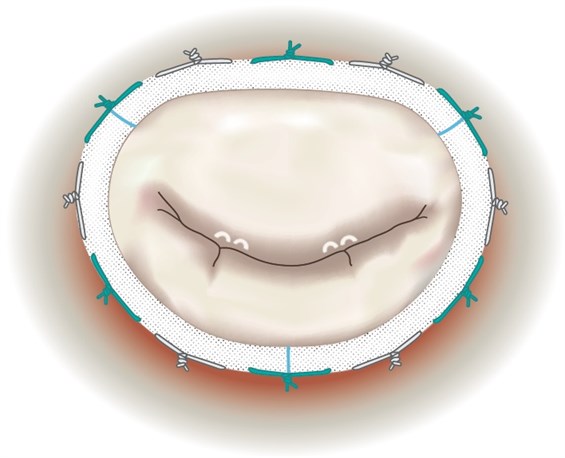 |
| Annuloplasty Ring Implanted to Support Repair with Sutures Conformed to Value Geometry |
What Are the Benefits of Minimally Invasive Mitral Valve Surgery?
- Reduced pain, blood loss and risk of infection
- Shorter hospital stay
- Faster recovery and return to work
- Less scarring and improved appearance after surgery

 "UCSF offers the full range of minimally invasive approaches for mitral valve repair and replacement using a small 4-6 cm incision. The benefits are significant including less post-operative pain at the incision site, a shorter hospital stay, a faster return to normal activities, and an improved cosmetic result."
"UCSF offers the full range of minimally invasive approaches for mitral valve repair and replacement using a small 4-6 cm incision. The benefits are significant including less post-operative pain at the incision site, a shorter hospital stay, a faster return to normal activities, and an improved cosmetic result."







