Atrial Fibrillation
Atrial fibrillation (A-tre-al fi-bri-LA-shun), or AF, is the most common type of arrhythmia (ah-RITH-me-ah). An arrhythmia is a problem with the rate or rhythm of the heartbeat. During an arrhythmia, the heart can beat too fast, too slow, or with an irregular rhythm.
AF occurs when rapid, disorganized electrical signals cause the atria (AY-tree-uh), the two upper chambers of the heart, to fibrillate. The term "fibrillate" means to contract very fast and irregularly.
In AF, blood pools in the atria and isn't pumped completely into the ventricles (VEN-trih-kuls), the heart's two lower chambers. As a result, the heart's upper and lower chambers don't work together as they should.
Often, people who have AF may not feel symptoms. However, even when not noticed, AF can increase the risk of stroke. In some people, AF can cause chest pain or heart failure, particularly when the heart rhythm is very rapid.
AF may occur rarely or every now and then, or it may become a persistent or permanent heart rhythm lasting for years.
Understanding the Heart's Electrical System
To understand AF, it helps to understand the heart's internal electrical system. The heart's electrical system controls the rate and rhythm of the heartbeat.
With each heartbeat, an electrical signal spreads from the top of the heart to the bottom. As the signal travels, it causes the heart to contract and pump blood. The process repeats with each new heartbeat.
Each electrical signal begins in a group of cells called the sinus node or sinoatrial (SA) node. The SA node is located in the right atrium. In a healthy adult heart at rest, the SA node fires off an electrical signal to begin a new heartbeat 60 to 100 times a minute. (This rate may be slower in very fit athletes.)
From the SA node, the electrical signal travels through the right and left atria. This causes the atria to contract and pump blood into the ventricles.
The electrical signal then moves down to a group of cells called the atrioventricular (AV) node, located between the atria and the ventricles. Here, the signal slows down just a little, allowing the ventricles time to finish filling with blood.
The electrical signal then leaves the AV node and travels to the ventricles. This causes the ventricles to contract and pump blood out to the lungs and the rest of the body. The ventricles then relax, and the heartbeat process starts all over again in the SA node.
For more information on the heart's electrical system and detailed animations, go to the Diseases and Conditions Index How the Heart Works article.
Understanding the Electrical Problem in Atrial Fibrillation
In AF, the heart's electrical signals don't begin in the SA node. Instead, they begin in another part of the atria or in the nearby pulmonary veins. The signals don't travel normally, and they may spread throughout the atria in a rapid, disorganized way. This can cause the atria to fibrillate.
The abnormal electrical signals flood the AV node with electrical impulses. As a result, the ventricles also begin to beat very fast. However, the AV node can't conduct the signals to the ventricles as fast as they arrive. So, even though the ventricles may be beating faster than normal, they aren't beating as fast as the atria.
Thus, the atria and ventricles no longer beat in a coordinated way. This creates a fast and irregular heart rhythm. In AF, the ventricles may beat 100 to 175 times a minute, in contrast to the normal rate of 60 to 100 beats a minute.
When this happens, blood isn't pumped into the ventricles as well as it should be. Also, the amount of blood pumped out of the ventricles to the body is based on the randomness of the atrial beats.
The body may get rapid, small amounts of blood and occasional larger amounts of blood. The amount will depend on how much blood has flowed from the atria to the ventricles with each beat.
Most of the symptoms of AF are related to how fast the heart is beating. If medicines or age slow the heart rate, the symptoms are minimized.
AF may be brief, with symptoms that come and go and end on their own. Or, the condition may be persistent and require treatment. Sometimes AF is permanent, and medicines or other treatments can't restore a normal heart rhythm.
The animation below shows atrial fibrillation. Click the "start" button to play the animation. Written and spoken explanations are provided with each frame. Use the buttons in the lower right corner to pause, restart, or replay the animation, or use the scroll bar below the buttons to move through the frames.
The animation shows how the heart's electrical signal begins in a place other than the sinoatrial node, causing the atria to beat very fast and irregularly.
Outlook
People who have AF can live normal, active lives. For some people, treatment can cure AF and restore normal heart rhythms.
For people who have permanent AF, treatment can successfully control symptoms and prevent complications. Treatments include medicines, medical procedures, and lifestyle changes.
Types of Atrial Fibrillation
Paroxysmal Atrial Fibrillation
In paroxysmal (par-ok-SIZ-mal) atrial fibrillation (AF), the abnormal electrical signals and rapid heart rate begin suddenly and then stop on their own. Symptoms can be mild or severe and last for seconds, minutes, hours, or days.
Persistent Atrial Fibrillation
Persistent AF is a condition in which the abnormal heart rhythm continues until it's stopped with treatment.
Permanent Atrial Fibrillation
Permanent AF is a condition in which a normal heart rhythm can't be restored with the usual treatments. Both paroxysmal and persistent AF may become more frequent and, over time, result in permanent AF.
Other Names for Atrial Fibrillation
- A fib
- Auricular fibrillation
What Causes Atrial Fibrillation?
Atrial fibrillation (AF) occurs when the electrical signals traveling through the heart are conducted abnormally and become very rapid and disorganized.
This is the result of damage to the heart's electrical system. The damage most often is the result of other conditions, such as coronary heart disease (also called coronary artery disease) or high blood pressure, that affect the health of the heart.
Sometimes, the cause of AF is unknown.
Who Is At Risk for Atrial Fibrillation?
More than 2 million people in the United States have atrial fibrillation (AF). It affects both men and women.
The risk of AF increases as you age. This is mostly because as you get older, your risk for heart disease and other conditions that can cause AF also increases. However, about half of the people who have AF are younger than 75.
AF is uncommon in children.
Major Risk Factors
AF is more common in people who have heart diseases or conditions, such as:
- Coronary heart disease
- Heart failure
- Rheumatic heart disease
- Structural heart defects, such as mitral valve disorders
- Pericarditis (a condition in which the membrane, or sac, around your heart is inflamed)
- Congenital heart defects
- Sick sinus syndrome (a condition in which the heart's electrical signals don't fire properly and the heart rate slows down; sometimes the heart will switch back and forth between a slow rate and a fast rate)
AF also is more common in people who are having heart attacks or who have just had surgery.
Other Risk Factors
Other conditions that increase AF risk include hyperthyroidism (too much thyroid hormone), obesity, high blood pressure, diabetes, and lung disease.
Other factors also can increase your risk of AF. For example, drinking large amounts of alcohol, especially binge drinking, increases your risk. Even modest amounts of alcohol can trigger AF in some people. Caffeine or psychological stress also may trigger AF in some people.
Some evidence suggests that people who have sleep apnea are at greater risk for AF. Sleep apnea is a common disorder in which you have one or more pauses in breathing or shallow breaths while you sleep.
Metabolic syndrome also increases your risk of AF. People who have this condition have a group of risk factors that increase their risk of heart disease and other health problems.
Recent research suggests that people who receive high-dose steroid therapy are at increased risk of AF. This therapy, which is commonly used for asthma and certain inflammatory conditions, may act as a trigger in people who already have other AF risk factors.
What Are the Signs and Symptoms of Atrial Fibrillation?
Atrial fibrillation (AF) usually causes the ventricles to contract faster than normal. When this happens, the ventricles don't have enough time to fill completely with blood to pump to the lungs and body.
This inefficient pumping can cause signs and symptoms, such as:
- Palpitations (feelings that your heart is skipping a beat, fluttering, or beating too hard or fast)
- Shortness of breath
- Weakness or difficulty exercising
- Chest pain
- Dizziness or fainting
- Fatigue (tiredness)
- Confusion
Atrial Fibrillation Complications
AF has two major complications- stroke and heart failure.
Stroke
During AF, the atria don't pump all of their blood to the ventricles. Some blood pools in the atria. When this happens, a blood clot (also called a thrombus) can form.
If the clot breaks off and travels to the brain, it can cause a stroke. (A clot that forms in one part of the body and travels in the bloodstream to another part of the body is called an embolus.)
Blood-thinning medicines to reduce the risk of stroke are a very important part of treatment for people who have AF.
Atrial Fibrillation and Stroke
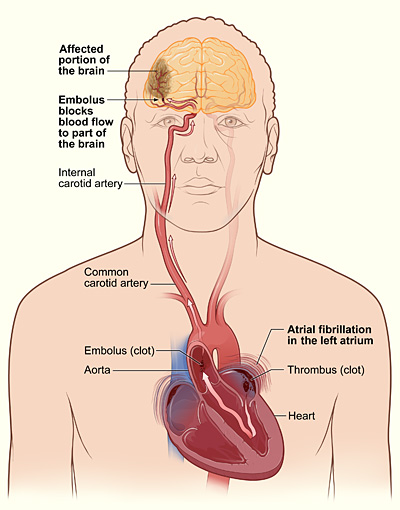
The illustration shows how a stroke can occur during atrial fibrillation. If a clot (thrombus) forms in the left atrium of the heart, a piece of it can dislodge and travel to an artery in the brain, blocking blood flow through the artery. The lack of blood flow to the portion of the brain fed by the artery causes a stroke.
Heart Failure
Heart failure occurs when the heart can't pump enough blood to meet the body's needs. AF can lead to heart failure because the ventricles are beating very fast and aren't able to properly fill with blood to pump out to the body.
Fatigue and shortness of breath are common symptoms of heart failure. A buildup of fluid in the lungs causes these symptoms. Fluid also can build up in the feet, ankles, and legs, causing weight gain.
Lifestyle changes, medicines, and sometimes special care (rarely, a mechanical heart pump or heart transplant) are the main treatments for heart failure.
How Is Atrial Fibrillation Diagnosed?
Some people who have atrial fibrillation (AF) don't have symptoms. For these people, AF often is found during a physical exam or EKG (electrocardiogram) test done for another purpose. Other times, AF is diagnosed after a person goes to the doctor because of symptoms.
To understand why a person has AF and the best way to treat it, the doctor will want to find any immediate or underlying causes of the condition.
Doctors use several methods to diagnose AF, including taking medical and family histories, doing a physical exam, and doing several tests and procedures.
Specialists Involved
A primary care doctor often is involved in the initial diagnosis and treatment of AF. These doctors can include family practitioners and internists.
Doctors who specialize in the diagnosis and treatment of heart disease also may be involved, such as:
- Cardiologists. These are doctors who diagnose and treat heart diseases and conditions.
- Electrophysiologists. These are cardiologists who specialize in arrhythmias.
Medical and Family Histories
Your doctor will ask questions about your:
- Signs and symptoms. What symptoms are you having? Have you had palpitations? Are you dizzy or short of breath? Are your feet or ankles swollen (a possible sign of heart failure)? Do you have any chest pain?
- Medical history. This includes other health problems, such as a history of heart disease, high blood pressure, lung disease, diabetes, or thyroid problems.
- Family's medical history. Does anyone in your family have a history of AF? Has anyone in your family ever had heart disease or high blood pressure? Has anyone had thyroid problems? Are there other illnesses or health problems in your family?
- Health habits. Your doctor may ask whether you smoke or use alcohol or caffeine.
Physical Exam
Your doctor will do a complete cardiac exam, listening to the rate and rhythm of your heartbeat and taking your pulse and blood pressure reading. He or she will likely check to see whether you have any signs of heart muscle or valve problems. Your doctor will listen to your lungs to check for signs of heart failure.
Your doctor also will check for swelling in your legs or feet and look for an enlarged thyroid gland or other signs of hyperthyroidism (too much thyroid hormone).
Diagnostic Tests and Procedures
EKG
An EKG is a simple, painless test that records the heart's electrical activity. It's the most useful test for diagnosing AF.
An EKG shows how fast your heart is beating and its rhythm (steady or irregular). It also records the strength and timing of electrical signals as they pass through each part of your heart.
A standard EKG only records the heartbeat for a few seconds. It won't detect an AF episode that doesn't happen during the test. To diagnose paroxysmal AF, your doctor may ask you to wear a portable EKG monitor that can record your heartbeat for longer periods.
The two most common types of portable EKGs are Holter and event monitors.
Holter and Event Monitors
A Holter monitor records the heart's electrical activity for a full 24- or 48-hour period. You wear small patches called electrodes on your chest. These patches are connected by wires to a small, portable recorder. The recorder can be clipped to a belt, kept in a pocket, or hung around your neck.
You wear the Holter monitor while you do your normal daily activities. This allows the monitor to record your heart for a longer time than a standard EKG.
An event monitor is similar to a Holter monitor. You wear an event monitor while doing your normal activities. However, an event monitor only records your heart's electrical activity at certain times while you're wearing it.
For many event monitors, you push a button to start the monitor when you feel symptoms. Other event monitors start automatically when they sense abnormal heart rhythms.
You might wear an event monitor for 1 to 2 months, or as long as it takes to get a recording of your heart during symptoms.
Stress Test
Some heart problems are easier to diagnose when your heart is working hard and beating fast. During stress testing, you exercise (or are given medicine if you're unable to exercise) to make your heart work hard and beat fast while heart tests are done.
Echocardiography
Echocardiography (echo) uses sound waves to create a moving picture of your heart. The test provides information about the size and shape of your heart and how well your heart chambers and valves are working.
Echo also can identify areas of poor blood flow to the heart, areas of heart muscle that aren't contracting normally, and previous injury to the heart muscle caused by poor blood flow.
This test is sometimes called transthoracic (trans-thor-AS-ik) echocardiography. It's painless and noninvasive (no instruments are inserted into the body). The test is done by placing a device called a transducer on your chest. The device sends special sound waves through your chest wall to your heart.
The sound waves bounce off the structures of your heart, and a computer converts them into pictures on a screen.
Transesophageal Echocardiography
Transesophageal (trans-e-SOF-ah-ge-al) echo, or TEE, takes pictures of your heart through the esophagus (the passage leading from your mouth to your stomach).
The atria are deep in your chest and often can't be seen very well using transthoracic echo. Your doctor can see the atria much better using TEE.
During this test, the transducer is attached to the end of a flexible tube that's guided down your throat and into your esophagus. You'll probably be given medicine to help you relax during the procedure. TEE is used to detect blood clots that may be developing in the atria because of AF.
Chest X Ray
A chest x ray is a painless test that creates pictures of the structures in your chest, such as your heart and lungs. This test can show fluid buildup in the lungs and other complications of AF.
Blood Tests
Blood tests check the level of thyroid hormone and the balance of your body's electrolytes. Electrolytes are minerals that help maintain fluid levels and acid-base balance in the body. They're essential for normal health and functioning of your body's cells and organs.
How Is Atrial Fibrillation Treated?
Treatment for atrial fibrillation (AF) depends on how severe or frequent the symptoms are and whether you already have heart disease. General treatment options include medicines, medical procedures, and lifestyle changes.
Goals of Treatment
The goals of treating AF include:
- Preventing blood clots from forming, thereby reducing the risk of stroke.
- Controlling how many times a minute the ventricles contract. This is called rate control. Rate control is important because it allows the ventricles enough time to completely fill with blood. With this approach, the irregular heart rhythm continues, but the person feels better and has fewer symptoms.
- Restoring a normal heart rhythm. This is called rhythm control. Rhythm control allows the atria and ventricles to work together to efficiently pump blood to the body.
- Treating any underlying disorder that's causing or raising the risk of AF-for example, hyperthyroidism (too much thyroid hormone).
Who Needs Treatment for Atrial Fibrillation?
People who have AF but don't have symptoms or related heart problems may not need treatment. AF may even go back to a normal heart rhythm on its own. (This also can occur in people who have AF with symptoms.)
In some people who have AF for the first time, doctors may choose to use an electrical procedure or medicine to restore the heart rhythm to normal.
Repeated episodes of AF tend to cause changes to the heart's electrical system, leading to persistent or permanent AF. Most people who have persistent or permanent AF need treatment to control their heart rates and prevent complications.
Specific Types of Treatment
Blood Clot Prevention
The risk of a blood clot traveling from the heart to the brain and causing a stroke is increased in people who have AF. Preventing blood clots from forming is probably the most important part of treating AF.
Doctors prescribe blood-thinning medicines to prevent blood clots. These medicines include warfarin (Coumadin®), heparin, and aspirin.
Warfarin is the most effective medicine in people who have risk factors for stroke. People taking warfarin must have regular blood tests to check how well the medicine is working.
Rate Control
Doctors prescribe medicines to slow down the rate at which the ventricles are beating. These medicines help bring the heart rate to a normal level.
Rate control is the recommended treatment for most patients who have AF, even though an abnormal heart rhythm continues and the heart doesn't work as well as it should. Most people feel better and can function well if their heart rates are well-controlled.
Medicines used to control the heart rate include beta blockers (for example, metoprolol and atenolol), calcium channel blockers (diltiazem and verapamil), and digitalis (digoxin). Several other medicines also are available.
Rhythm Control
Doctors use medicines or procedures to restore and maintain the heart's rhythm. This treatment approach is recommended for people who aren't functioning well with rate control treatment or who have only recently started having AF.
The longer you have AF, the less likely it is that an abnormal heart rhythm can be restored to a normal heart rhythm. This is especially true for people who have had AF for 6 months or more.
Restoring a normal rhythm also becomes less likely if the atria become enlarged or if any underlying heart disease becomes more severe. In these cases, the chance that AF will recur is high, even if you're taking medicine to help convert AF to a normal rhythm.
Medicines. Medicines used to control the heart rhythm include amiodarone, sotalol, flecainide, propafenone, dofetilide, and ibutilide. Occasionally, older medicines, such as quinidine, procainamide, and disopyramide, are used.
Your doctor will carefully tailor the dose and type of medicines he or she prescribes to treat your AF. This is because medicines used to treat AF can cause a different kind of arrhythmia. They also can harm people who have underlying diseases of the heart or other organs. This is particularly true for patients who have an unusual heart rhythm problem called Wolff-Parkinson-White syndrome.
Your doctor may start you on a small dose of medicine and then gradually increase the dose until your symptoms are controlled. Medicines used for rhythm control can be given regularly by injection at a doctor's office, clinic, or hospital. Or, you may routinely take pills to try to control AF or prevent recurrences.
If your doctor knows how you'll react to a medicine, a specific dose may be prescribed for you to take on an as-needed basis if you have an episode of AF.
Procedures. Doctors use several procedures to restore a normal heart rhythm. Electrical cardioversion is a procedure used to restore a fast or irregular heartbeat to a normal rhythm. For the procedure, low-energy shocks are given to your heart to trigger a normal rhythm. You're temporarily put to sleep before the shocks are given.
Electrical cardioversion isn't the same as the emergency heart shocking procedure often seen on TV programs. It's planned in advance and done under carefully controlled conditions.
Before doing electrical cardioversion, your doctor may recommend transesophageal echocardiography (TEE) to rule out the presence of blood clots in the atria. If clots are present, you may need to take blood-thinning medicines for a period of time to help get rid of the clots before the procedure.
Catheter ablation may be used to restore a normal heart rhythm when medicines or electrical cardioversion don't work. During this procedure, a wire is inserted through a vein in the leg or arm and threaded to the heart.
Radio wave energy is sent through the wire to destroy abnormal tissue that may be disrupting the normal flow of electrical signals. An electrophysiologist usually does this procedure in a hospital.
Sometimes catheter ablation is used to destroy the atrioventricular (AV) node. The AV node is where the heart's electrical signals pass from the atria to the ventricles. This procedure requires your doctor to surgically implant a device called a pacemaker to maintain a normal heart rhythm.
Research to examine the benefits of catheter ablation as a treatment for AF is still ongoing.
Another procedure to restore a normal heart rhythm is called "maze" surgery. During this procedure, the surgeon makes small cuts or burns in the atria that prevent the spread of disorganized electrical signals.
This procedure requires open-heart surgery, so it's usually done when a person requires heart surgery for other reasons, such as for valve disease (which can increase the risk of AF).
Approaches To Treating Underlying Causes and Reducing Risk Factors
Your doctor also may recommend other treatments for an underlying condition that may be causing AF or to reduce AF risk factors. For example, he or she may prescribe medicines to treat an overactive thyroid or reduce blood pressure.
Your doctor also may recommend lifestyle changes, such as following a healthy diet, cutting back salt intake (to help lower blood pressure), quitting smoking, and reducing stress.
Limiting or avoiding stress and alcohol, caffeine, or other stimulants that may increase your heart rate also may help reduce the risk of AF.
How Can Atrial Fibrillation Be Prevented?
You may be able to prevent atrial fibrillation (AF) by following a healthy lifestyle and taking steps to lower your risk of heart disease. These steps include:
- Following a heart healthy diet that's low in saturated fat, trans fat, and cholesterol. A healthy diet includes a variety of whole grains, fruits, and vegetables daily.
- Not smoking.
- Getting physical activity regularly.
- Maintaining a healthy weight.
If you have heart disease or other AF risk factors, work with your doctor to control your condition and lower your risk of complications, such as AF.
In addition to following the healthy lifestyle steps above, which also can help control heart disease, your doctor may advise you to take one or more of the following steps:
- Follow the DASH eating plan to help lower your blood pressure.
- Keep your cholesterol and triglycerides at healthy levels with dietary changes and/or medicines.
- Limit or avoid alcohol.
- Control your blood glucose (blood sugar) levels if you have diabetes.
- Get ongoing medical care and take your medicines as prescribed.
For more information about following a healthy lifestyle, visit the National Heart, Lung, and Blood Institute's Aim for a Healthy Weight Web site, "Your Guide to a Healthy Heart," "Your Guide to Lowering Your Blood Pressure With DASH," and "Your Guide to Physical Activity and Your Heart."
Living With Atrial Fibrillation
People who have atrial fibrillation (AF)-even permanent AF-can live normal, active lives. If you have AF, ongoing medical care is important.
Keep all your medical appointments. Bring all the medicines you're taking to every doctor and emergency room visit. This will help your doctor know exactly what medicines you're taking.
Follow your doctor's instructions for taking medicines. Be careful about taking over-the-counter medicines, nutritional supplements, and cold and allergy medicines. Some of these products contain stimulants that can trigger rapid heart rhythms. Some over-the-counter medicines can have harmful interactions with heart rhythm medicines.
Tell your doctor if your medicines are causing side effects, if your symptoms are getting worse, or if you have new symptoms.
If you're taking blood-thinning medicines, you'll need to be carefully monitored. For example, you may need regular blood tests to check how the medicines are working.
Talk with your doctor about diet, physical activity, weight control, and alcohol use. Find out what steps you can take to manage your condition.
Key Points
- Atrial fibrillation (AF) is the most common type of arrhythmia. An arrhythmia is a problem with the rate or rhythm of the heartbeat.
- AF occurs when rapid, disorganized electrical signals cause the atria to fibrillate (contract very fast and irregularly). When this happens, the heart's upper and lower chambers don't work together as they should.
- Often, people who have AF may not feel symptoms. However, even when not noticed, AF can increase the risk of stroke. In many people, AF can cause chest pain or heart failure, particularly when the heart rhythm is rapid.
- The three types of AF are paroxysmal (the AF comes and goes), persistent (the AF continues until stopped with treatment), and permanent (a normal heart rhythm can't be restored).
- Certain conditions, such as coronary heart disease or problems with the heart's structure, can lead to AF. Other conditions, such as obesity and high blood pressure, make it more likely that an episode of AF will happen.
- More than 2 million people in the United States have AF. It's affects both men and women. The risk of AF increases as you age.
- Signs and symptoms of AF include palpitations, shortness of breath, weakness or difficulty exercising, chest pain, dizziness or fainting, fatigue (tiredness), or confusion.
- AF has two major complications-stroke and heart failure. In AF, blood pools in the atria and isn't pumped completely into the ventricles. As a result, blood clots can form in the atria. A stroke can occur if a blood clot in the atria breaks off and travels through the bloodstream to the brain. Heart failure can occur because the heart isn't able to function well and pump enough blood to the rest of the body.
- Doctors diagnose AF using medical and family histories, a physical exam, and tests and procedures. The most useful test for diagnosing AF is an EKG (electrocardiogram).
- Treatment for AF depends on how severe or frequent the symptoms are and whether you already have heart disease. General treatment options include medicines, medical procedures, and lifestyle changes.
- You may be able to prevent AF by following a heart healthy lifestyle and taking steps to lower your risk of heart disease, such as following a healthy diet, not smoking, getting physical activity regularly, and maintaining a healthy weight.
- People who have AF can live normal, active lives. For some people, treatment can cure AF and return their heartbeats to normal rhythms. For people who have permanent AF, treatment can successfully control symptoms and prevent complications.







